Orthopedic EMR
#1 Orthopedic EMR & PM
AllegianceMD Veracity Orthopedic EMR is #1 among Orthopedic specialists.
Mesenchymal Stem Cell Therapy for Degenerative Disc Disease: A Comprehensive Overview for Orthopedic Surgeons
Abstract:
Degenerative disc disease (DDD) is a leading cause of chronic low back pain (LBP) and disability worldwide, imposing substantial socioeconomic burdens on healthcare systems. With limited efficacy and durability of current conservative and surgical treatments, regenerative strategies—especially mesenchymal stem cell (MSC) therapy—have garnered significant interest. This article provides a detailed review of the pathophysiological underpinnings of DDD, the biological rationale for MSC interventions, and the clinical data supporting their use in orthopedic practice. Particular emphasis is placed on patient selection, procedural techniques, and the regulatory and practical challenges that clinicians must navigate.
1. Introduction
Low back pain is the most common musculoskeletal complaint, affecting up to 80% of adults at some point in their lives 1,2. Among the many etiologies of LBP, degenerative disc disease plays a central role, driven by structural and biochemical alterations that compromise the intervertebral disc’s integrity. While non-surgical management and spine surgery can offer symptom relief, these approaches do not directly address the restoration of disc tissue. Consequently, biologic therapies—particularly mesenchymal stem cell (MSC) therapy—have emerged as a promising strategy to potentially reverse or halt degenerative processes 3.
2. Pathophysiology of Degenerative Disc Disease
2.1 Disc Anatomy and Aging
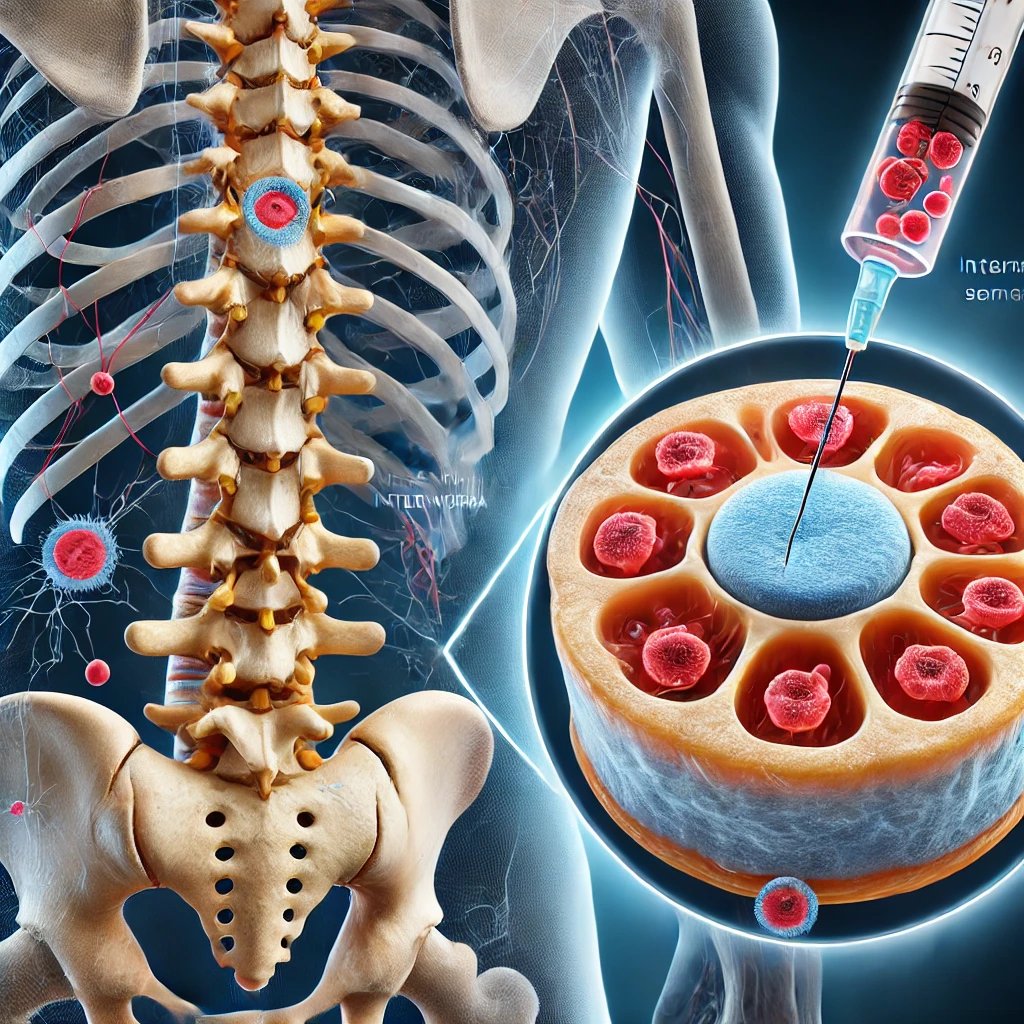
The intervertebral disc comprises the outer annulus fibrosus (AF), the central nucleus pulposus (NP), and cartilaginous endplates. The NP is rich in proteoglycans and type II collagen, conferring high water-binding capacity essential for load-bearing. With aging or mechanical injury, proteoglycan content declines, water retention decreases, and microfissures develop in the AF 4. These changes reduce disc height, alter load distribution, and predispose to neural ingrowth and pain.
2.2 Inflammatory Cascade
Pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-6, along with matrix metalloproteinases (MMPs), drive a vicious cycle of disc matrix degradation and local inflammation 5. The resultant inflammatory microenvironment contributes to nociceptive signaling and can exacerbate LBP. This pathophysiological backdrop underscores the potential utility of MSCs, which can modulate inflammation and support extracellular matrix repair.
3. Mesenchymal Stem Cell Therapy: Mechanisms of Action
3.1 Differentiation Potential
MSCs, derived from sources including bone marrow, adipose tissue, and umbilical cord blood, possess multipotent capability. Under appropriate conditions, they can differentiate into chondrocytes, which are integral for proteoglycan synthesis and maintenance of disc structure 6.
3.2 Paracrine Activity and Immunomodulation
Beyond differentiation, MSCs secrete a host of growth factors (e.g., TGF-β, IGF-1) and anti-inflammatory cytokines that can promote resident disc cell proliferation, dampen catabolic activity, and mitigate local inflammation 7. This paracrine effect may be critical for restoring an anabolic-catabolic balance in degenerating discs.
3.3 Low Immunogenicity
MSCs typically express low levels of major histocompatibility complex (MHC) antigens, reducing the risk of immune rejection. This immunoprivileged characteristic broadens the potential for both autologous and allogeneic therapies, although autologous MSCs remain the most widely investigated in orthopedic applications 8.
4. Sources and Preparation of MSCs
Bone Marrow (BM-MSCs):
Commonly harvested from the iliac crest using aspiration techniques.
Broad clinical experience and proven utility in cartilage and bone repair 9.
Adipose Tissue (AD-MSCs):
Obtained via liposuction. Higher yield but potentially less chondrogenic differentiation compared to BM-MSCs; however, data remains inconclusive 10.
Umbilical Cord & Placental Tissue:
Allogeneic sources providing “off-the-shelf” accessibility. Require stringent donor screening and Good Manufacturing Practice (GMP) processing 11.
Processing Methods:
Collected tissues undergo enzymatic digestion or centrifugation to isolate the MSC fraction. Cell expansion may occur in specialized laboratories to obtain sufficient cell counts. Flow cytometry is typically utilized to confirm MSC phenotypic markers (CD73, CD90, CD105), ensuring standardization and purity 12.
5. Current Clinical Evidence
5.1 Early-Phase Clinical Studies
Pettine et al. (2015): A pilot study assessing autologous MSC injections in DDD patients demonstrated a notable reduction in VAS pain scores and improvement in the Oswestry Disability Index (ODI). Follow-up MRI hinted at partial disc rehydration in several participants 13.
Noriega et al. (2017): Using autologous BM-MSCs, a pilot study reported significant improvements in pain and function at 12 months post-injection, with MRI evidence suggesting a slowdown in degenerative progression 14.
5.2 Systematic Reviews and Meta-Analyses
Wu et al. (2018): A systematic review of animal and human studies underscored the potential of MSCs to preserve disc structure and alleviate pain. However, heterogeneity in cell sources, preparation methods, and follow-up periods highlighted the need for larger, standardized trials 15.
Liang et al. (2022): A meta-analysis in Spine Journal confirmed short-term safety and efficacy of MSC injections for mild to moderate DDD but called for rigorous, long-term data to validate durability 16.
5.3 Ongoing Clinical Trials
Multiple Phase I/II randomized controlled trials (RCTs) are underway globally, exploring:
- Optimal Cell Dosages
- Scaffold or Carrier Materials
- Adjunct Growth Factors
These studies aim to refine protocols, reduce variability, and better characterize the long-term safety profile of MSC therapy 17.
6. Procedure and Technical Considerations
Patient Selection
- MRI or CT confirmation of DDD without significant spinal instability or deformity.
- Chronic discogenic pain refractory to conservative care.
- Appropriate psychosocial screening to identify potential confounders (e.g., depression, secondary gain).
Injection Technique
- Percutaneous approach under fluoroscopy or CT guidance.
- Target NP region with precise needle placement.
- Employ stringent sterile techniques to mitigate infection risk 18.
Post-Injection Protocols
- Initial phase of restricted axial loading to promote cell engraftment.
- Gradual reintroduction of physical therapy and core stabilization exercises.
Safety Profile
- Minimal immediate complications: localized pain, soreness, or transient inflammatory response.
- Rare events: infection, allergic or immune reaction (especially with allogeneic cells).
- No confirmed malignant transformation in short- to mid-term follow-up; ongoing vigilance is warranted 19.
7. Challenges and Limitations
Heterogeneity in Cell Products:
Variations in tissue source, isolation protocols, and expansion conditions complicate direct comparisons across studies.
Regulatory Framework:
Agencies such as the FDA (USA) and EMA (Europe) impose stringent regulations on cell-based therapies, requiring GMP-compliant processing and clear evidence of safety and efficacy 20.
Cost and Insurance Coverage:
MSC therapy is often labeled experimental, limiting reimbursement and necessitating out-of-pocket expenses for patients. Economic analyses are needed to evaluate cost-effectiveness at scale.
Long-Term Durability:
While pilot studies and short-term follow-ups are encouraging, robust RCT data extending beyond 2–5 years are necessary to validate sustained clinical benefit.
8. Future Directions
Cellular Enhancements:
- Genetic Engineering (e.g., CRISPR): Tailoring MSCs for enhanced cartilage-like matrix production.
- Preconditioning: Hypoxic or mechanical stimuli in vitro to boost MSC viability and engraftment post-injection.
Combination Strategies:
- Biocompatible Scaffolds: Improve MSC retention and guide neotissue organization.
- Adjunct Biologics: Growth factors, platelet-rich plasma, or exosomes to further stimulate regenerative responses.
Personalized Medicine Approaches:
- Integrating patient genomic profiles and molecular biomarkers to customize MSC therapies for optimal outcomes.
- Potential synergy with advanced imaging techniques (e.g., T2 mapping, quantitative MRI) to track disc regeneration in real time.
9. The Role of Orthopedic Electronic Health Records (EHR) in MSC Therapy for DDD
Electronic Health Records (EHR) systems can play a pivotal role in advancing the application of mesenchymal stem cell (MSC) therapy for degenerative disc disease (DDD). By integrating patient data, streamlining workflows, and facilitating research, EHRs can enhance both clinical and operational outcomes. Below are key ways EHRs can support MSC therapy:
9.1 Enhanced Patient Selection and Data Integration
EHRs enable clinicians to consolidate patient data, including medical history, imaging results (e.g., MRI, CT), and prior treatments, into a single platform. This comprehensive view aids in identifying suitable candidates for MSC therapy by ensuring that only patients with confirmed DDD and no contraindications are selected. Additionally, EHRs can flag patients who have failed conservative treatments, streamlining the referral process for regenerative therapies.
9.2 Tracking Treatment Outcomes
EHRs can be used to systematically track patient outcomes following MSC therapy. By documenting pain scores (e.g., VAS), functional improvements (e.g., Oswestry Disability Index), and imaging findings over time, clinicians can monitor the efficacy of the treatment. This longitudinal data collection is critical for evaluating the durability of MSC therapy and identifying factors that influence success.
9.3 Facilitating Research and Clinical Trials
EHRs can serve as a valuable tool for conducting research and clinical trials. By aggregating de-identified patient data, researchers can analyze trends, identify predictors of treatment success, and compare outcomes across different MSC sources or protocols. EHRs also simplify the recruitment process for clinical trials by identifying eligible patients based on predefined criteria.
9.4 Improving Care Coordination
MSC therapy often involves a multidisciplinary team, including orthopedic surgeons, radiologists, physical therapists, and pain management specialists. EHRs facilitate seamless communication and coordination among these providers by providing real-time access to patient records, treatment plans, and progress notes. This ensures that all team members are aligned and can deliver personalized, cohesive care.
9.5 Regulatory Compliance and Documentation
Given the stringent regulatory requirements for cell-based therapies, EHRs can help ensure compliance by maintaining detailed records of MSC sourcing, processing, and administration. Automated documentation features can reduce the administrative burden on clinicians while ensuring that all regulatory standards are met.
9.6 Cost and Resource Optimization
EHRs can provide insights into the cost-effectiveness of MSC therapy by tracking resource utilization, patient outcomes, and long-term benefits. This data can inform decision-making and help justify the use of MSC therapy to insurers and healthcare administrators.
10. Conclusion
Mesenchymal stem cell therapy for degenerative disc disease represents a significant leap toward biologically restoring disc integrity and reducing the chronic pain burden. Early clinical evidence shows promise, with studies indicating pain relief, improved function, and possible partial disc rehydration. Nevertheless, large-scale, high-quality RCTs with standardized protocols and extended follow-up durations are essential to confirm long-term safety and efficacy. Orthopedic surgeons, alongside spine specialists and regenerative medicine researchers, stand at the forefront of translating this promising therapy into routine clinical practice—bringing the field closer to an era of truly regenerative spine care.
References
- Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81.
- Andersson GB. Epidemiological features of chronic low-back pain. Lancet. 1999;354(9178):581-585.
- Freemont AJ. The cellular pathobiology of the degenerating intervertebral disc and discogenic back pain. Rheumatology (Oxford). 2009;48(1):5-10.
- Urban JP, Roberts S. Degeneration of the intervertebral disc. Arthritis Res Ther. 2003;5(3):120-130.
- Le Maitre CL, Hoyland JA, Freemont AJ. Catabolic cytokine expression in degenerate and herniated human intervertebral discs: IL-1β and TNFα expression profile. Arthritis Res Ther. 2007;9(4):R77.
- Caplan AI. Mesenchymal stem cells. J Orthop Res. 1991;9(5):641-650.
- Stagg J, Galipeau J. Mechanisms of immune modulation by mesenchymal stem cells and clinical translation. Curr Mol Med. 2013;13(5):856-867.
- Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8(9):726-736.
- Hernigou P, Poignard A, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Influence of the number and concentration of progenitor cells. J Bone Joint Surg Am. 2005;87(7):1430-1437.
- Ning H, Yang F, Jiang M, Hu L, Feng K, Zhang J. The correlation between the immunosuppressive effects of human adipose-derived stem cells and nitric oxide production. Biochem Biophys Res Commun. 2019;509(1):145-151.
- Beeravolu N, McKee C, Alamri A, et al. Isolation and characterization of mesenchymal stromal cells from human umbilical cord and fetal placenta. J Vis Exp. 2017;(122):55326.
- Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315-317.
- Pettine DS, Murphy MB, Suzuki RK, Sand TT. Safety and Feasibility of Treating Degenerative Disc Disease With an Autologous Mesenchymal Stem Cell Injection: A Pilot Study. Tissue Eng Part A. 2015;21(3-4):384-390.
- Noriega DC, Ardura F, Hernández-Ramajo R, et al. Intervertebral Disc Repair by Autologous Mesenchymal Bone Marrow Cells: A Pilot Study. Transplantation. 2017;101(8):1945-1951.
- Wu T, Song HX, Dong Y, et al. Efficacy of mesenchymal stem cells in intervertebral disc repair: a systematic review and meta-analysis of animal controlled trials. Arthritis Res Ther. 2018;20(1):153.
- Liang H, Li Z, Wei T, et al. Mesenchymal stem cell transplantation for degenerative disc disease: a meta-analysis of clinical and preclinical data. Spine J. 2022;22(6):876-888.
- Vadala G, Russo F, Ambrosio L, Loppini M, Papalia R, Denaro V. Stem cells sources for intervertebral disc regeneration. World J Stem Cells. 2016;8(9):185-201.
- Grunert P, Hudson KD, MacDowell A, et al. Assessment of intervertebral disc height in single- and multilevel lumbar disc herniation procedures using fluoroscopic guidance: a technical note. J Neurosurg Spine. 2013;19(6):673-678.
- Centeno CJ, Busse D, Kisiday J, et al. Increased knee cartilage volume in degenerative joint disease using percutaneously implanted autologous mesenchymal stem cells. Pain Physician. 2008;11(3):343-353.
- Sensebé L, Gadelorge M, Fleury-Cappellesso S. Production of mesenchymal stromal/stem cells according to good manufacturing practices: a review. Stem Cell Res Ther. 2013;4(3):66.
Disclosure and Disclaimer:
This article aims to provide an evidence-based overview and does not substitute for individualized clinical judgment. Orthopedic surgeons and spine specialists should remain updated with evolving clinical trial outcomes and regulatory guidelines to optimize the application of MSC therapy for degenerative disc disease.
EHR, Practice Management, Billing Solution, Patient Portal and Self Check-In Kiosk.